ZEISS CIRRUS HD-OCT
Technology

OCT is a modern non-invasive diagnostic method, first introduced into clinical practice in 1997, which examines tissues in vivo. It is based on complex analyses of the reflection of low-coherent radiation (parallel light rays enter the eye and are reflected differently depending on the condition of the tissue being examined and its pathological changes).
Promedica Ophthalmology has an Optical Coherence Tomograph model Cirrus HD OCT – Zeiss Meditek.
WHY CIRRUS OCT-ZEISS?
- Optical coherence tomography whose results are recognized for clinical trials.
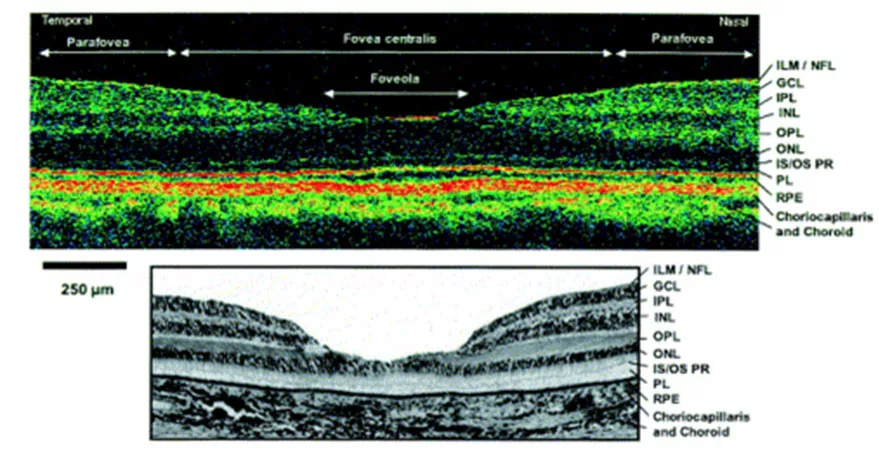
- High resolution that allows visualization of the retinal layers “in vivo”, similar to histological findings l.1
- There is software for both the anterior and posterior ocular segments.
- It has FDA (Food and Drug Administration) approval for the accuracy of data obtained for NFRL – neuroretinal fibrillary layer and for optic disc papilla scan (excavation assessment). OCT (anatomical) results for Glaucoma correlate with physiological changes determined by HFA-Humphery Field Analyzer (computer perimetry) only when 30% of the NFRL is destroyed (in practice, RNFL analysis provides the opportunity to see anatomical changes before physiological changes occur).
Structures that are analyzed in the posterior ocular segment are the following:
- Macula
- Optic disc (optic papilla)
- Retinal neurofibrillary tangle Retina
Structures that are analyzed from the anterior ocular segment:
- Cornea with the possibility of measuring central corneal thickness
- Iridocorneal angle
The device has an integrated database system for comparison (reference system) for macula and retinal neurofibrillary tangle examinations for patients between the ages of 17 and 72, inclusive.
PATHOLOGY WHERE OCT IS APPLIED:
- Macular hole and pseudohole
- Vitreoretinal surface lesions and vitreoretinal traction syndrome.
- Foveal retinoschisis
- Epiretinal membrane (macular pucker)
- Macular edema from various causes (post-vasoocclusive disease, diabetic macular edema, uveitic macular edema, etc.).
- Serous and hemorrhagic detachment of the retina and pigment epithelium
- Macular degeneration, juvenile and age-related
- Diabetic retinopathy
- Acute and chronic epitheliopathy
- Subretinal neovascularization
- Intraretinal and preretinal neovascularizations
- Retinal atrophy
- Glaucoma and its sequelae
OCT MAKES IT POSSIBLE TO DETECT AND MEASURE:
- Morphological changes
- Retinal thickness
- Retinal thickness and retinal neurofibrillary tangle
- Retinal volume
- Different parameters of the papilla disk
- Cross section of the iridocorneal angle
- Cross-section of the cornea with the possibility of measuring central corneal thickness (pachymetry).
THE RESULTS OBTAINED MAY BE:
- analyze
- quantify (express graphically with numbers and percentages)
- to be stored in the hard disk of the device itself, as well as to be extracted to an electronic medium (CD-ROM or floppy disk)
- to compare results over time (e.g. compare today’s results with results from a month ago for the same patient).
- Monitoring disease progression
- To quantify the lesions
- To do pharmaceutical or post-graduate studies
When can’t OCT be done?
- Significantly reduced visual acuity, inability of the patient to fixate, bilaterally.
- Opacity of optical media.
- It is contraindicated in people suffering from epilepsy.
- In young children (poor cooperation, low compliance).
WHY OCT?
- Non-invasive,
- Non-contact,
- Safe,
- Fast,
- Sensitive, high resolution.